Health care is always adapting and evolving and this has led to several modes for training future health care professionals. One of the most important evolutions in the curriculum development of this field is the introduction of simulation-based medical education and training.
Simulation is known as a generic term that describes an artificial representation of an actual world process to acquire educational goals through experiential learning. Medical education that is based on simulation is referred to as any educational activity that uses simulation aides to recreate clinical scenarios. Simulation has been brought in use for a long time in many high-risk professions such as Aviation but medical simulation is a relatively new term. Rather than an apprentice-style of learning, the acquisition of clinical skills through devoted practice is something that medical simulation allows. An alternative to real patients is simulation tools and with the help of these, a trainee can learn the medical techniques by making mistakes without the fear of harming the patient. There are various classifications and types of simulators and their cost varies depending upon the degree of their resemblance to the reality.
Simulation-based learning might be a little expensive but it is cost-effective if utilized properly. Medical simulation has been found to increase clinical competence at the UG and PG levels and also has been found with many advantages that can reduce health care costs by improving the medical provider’s competencies and enhance patient safety.
Purpose of Medical Simulation in Education
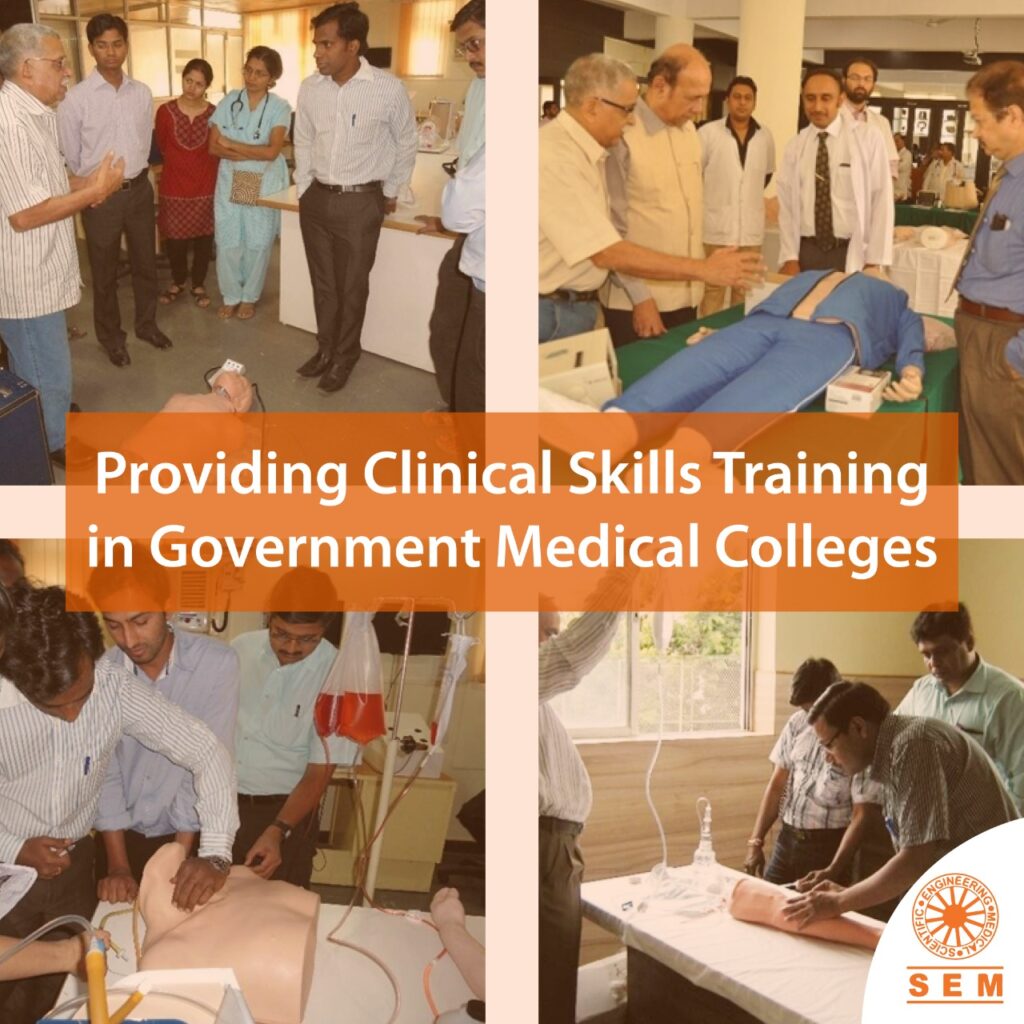
Clinical simulation has taken off as a performance improvement tool and training modality tool within health care, over the last 15 years. While in the medical field, traditional and older learning mechanisms like apprenticeships, lectures and practice-based learning still continue to offer the students the foundation knowledge that is required for the successful future, simulation-based learning and training have actually revolutionized medical education.
With the originations during a math experiment during World War 2, simulation technologies now have great applications in different industries ranging from entertainment to manufacturing to healthcare. Simulation tools have also found widespread advantages and successes in the field of education, being utilized for training, teaching and testing applications. As computer technology continues to evolve, simulations will become more involved and will continue to transform applications in the field of education.
Domains of Clinical Competence
The six domains of Clinical Competence establishing Basic Physician Competencies are:
- Patient Care
- Medical Knowledge
- Practice Based Learning and Improvement
- Interpersonal and Communication Skills
- Professionalism
- System based Practice.
Dr David Leach, M.D. Executive Director of the American Council for Graduate Medical Education (ACGME) has proposed that Simulation can help achieve our objectives in Resident Education as follows:
1: Enable the acquisition of skills by Residents in low stakes environment away from the Patient bedside.
2: Providing the means for Procedures, Treatments Rehearsals and Debriefings.
3: Serving as a “Formative Tool” for the Residents Development.
4: Helping to determine just, “How residents respond in different contexts”?
5: Exposing the mastery of both rules and values through the judicious use of improvisations
6: Populating a Portfolio of “Assessed Experiences’ that enable residents to demonstrate their abilities.
7: Permitting Residents to make deliberate errors, to learn about their consequences.
8: Helping Residents learn “System Based Practice” through Simulation, that involve “Multiple Interdependent Variables”
9: Documenting just, “How residents think” rather than simply “What they Think”
10: Expressing Respect in concrete demonstratable manner.
- The future of Medical Student Education, Resident Training and Maintenance of Competence and Clinical Privileges in Practice will , in the years to come bear very little resemblance to the past.
- Simulation, makes us accept the “Primacy of Patient Welfare” and makes us embrace our “Commitment to Professional Competence”.
Advantages of Medical Simulation in Education and Training
- Simulation helps and allows healthcare participants to learn from their mistakes and improve their skills.
- Medical trainees are able to have a greater understanding of all the consequences of their actions and how essential it is to prevent it from happening again.
- Feedback is generated for the users immediately and it helps them to get exactly what went right or wrong. They also know about the underlying effects and how they can improve the results.
- Individual healthcare learners and teams make use of what they have learned hands-on by applying their thinking skills through simulation. For example, this could be involving decision-making, knowledge-in-action procedures and effective communication during a situation. Basically, this allows the interaction of humans with their medical environment and exploration of different medical factors.
- Simulation-based learning can be set up at suitable locations, scenarios, times and repeated as often as required.
- Simulation can be done with the minimal establishment at hospitals and other medical facilities or it can be undertaken in impressively high technology simulation centres.
- Simulation-based learning can be personalized to suit healthcare beginners, intermediates, experts and even adapt to evolve to the learners changing skills.
- Simulators encourage motivation, deepen the process of learning and assist the medical novice to become a healthcare expert by providing a mechanism to generate an understanding from another medical participant’s perspective.
- Debriefing tools that include peer review and video feedback are some key features of the simulation education, training and learning strategy.
These are some advantages of medical simulation that shows how it is transforming medical education and training. Now, let’s discuss them in more detail.
Benefits of Medical Simulation
1: Training on Simulators can help foster a culture in which Clinicians feel comfortable critiquing their own performances.
2: Simulators help create “On Screen Scenarios with Tactile Realism” on demand e.g. VST Vascular Intervention Systems Training.
3: The Current generation of Medical Personnel and Learners are very comfortable with Computers and they take to Simulation and Virtual Reality with great ease.
4: As 3D Reality becomes more sophisticated, they will eventually replace even Manikins.
5: Simulators powerfully make you suspend “Disbelief” Even if the patient is not real, the agony of trying to save life is real.
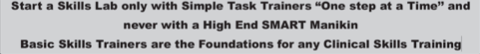
Suspending “Disbelief” is the key. Those undergoing training, must be able to feel and think as though they are performing within a real environment where their actions are associated with real consequences.
These training settings are not possible in classrooms which lack the multiple cues found in dynamic complex technical domains. Realism induces a sense of “Disbelief”. Suspension of Disbelief is a powerful factor in improving diagnostic skills and clinical judgments
Medical Simulation provides a novel and intermediate stage in Medical Education between “Classroom” and “Clinical Settings” and the factor of “Suspension of Disbelief” is a very important factor in integrating Simulation in traditional Medical Education and Continuing Medical Education
6: Research indicates that the optimal acquisition and retention of knowledge and skills by adults is achieved by active participation rather than by passive observations and helps improves diagnostic clinical skills and clinical judgments.
7: Professionals work in a dynamic domain, characterized by intense time pressures, unpredictable responses, complex communications patterns involving multiple personnel and high risks.
Successful operations within such dynamic domains requires the use of decision making skills, that are distinctly different from those required in relatively static domains such as clinical base medicine. Many training environments lack the features associated with such dynamic domains, thereby denying the professionals training within these environments, the opportunity to acquire and practice these unique decision making skills.
8: Many Medical Domains are as dynamic as in nature as the cockpit of a plane, and crisis arise much more frequently in Medicine than in Aviation and here Physicians are expected to make rapid and correct decisions in managing any Medical emergency.
9: The dynamic nature of the Delivery Room is similar to that of the Operating Room because many Neonatal Morbidities actually have their genesis in Utero.
10: Simulations are controlled environments in which multiple intense clinical experiences can be provided in a relatively brief period and these experiences can be scaled to fit the level of the trainee. The Simulator offers the convenience of scheduling and the option of repetition.
11: Trainees can learn to actively demonstrate appropriate technical and behavioral skills and they cannot simply talk their way through difficult scenarios
12: The use of video records provides an objective time coded record of “Trainee Communications and Actions” and creates a powerful stimulus for learning during facilitated debriefings.
13: Because the activities on the Simulator pose no risks to patients or to professional liability, the trainees are allowed to witness the “natural evolution” of mistakes without the need of intervention by senior faculty.
14: Simulators reduce the use of Hospital resources by supplanting expensive patient care areas as the location for clinical teaching and then recycling supplies and devices that normally would require disposal if used on real patients.
15: The use of real Medical equipments. Sophisticated Patient Simulators, High quality Audio-Video recording and playback systems and faculty with expertise, both in Medical and Educational aspects of Simulation based Training is more expensive in comparison to traditional training programs. However, experience indicates that the more realistic the Simulation, the greater the suspension of disbelief and more effective the training.
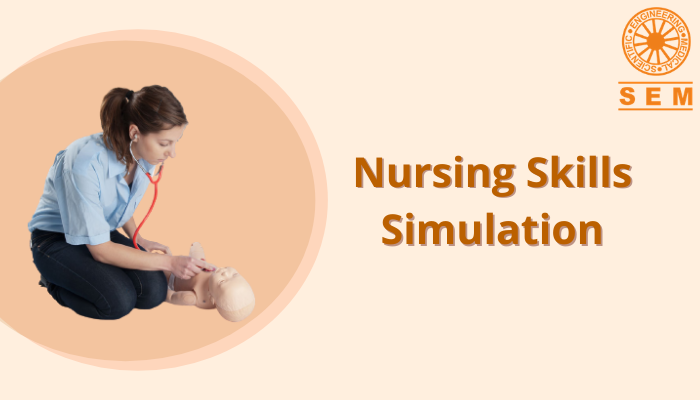
Working with Mannequins, gives the students a greater “genuine” experience as compared to working in a “Bedside training” with a tangible real patient.
16: Patient Safety has rapidly risen to the top of the Healthcare Policy and has been incorporated into Quality Initiatives. The unnecessary need for “Patient Risk” in “On-the-job training” diminishes as alternative but more realistic ways are developed to replicate “hospital situations”
17: Demand and transfer for curricula in Patient Safety and transfer of Safety lesions learnt in other risk laden industries, has created new responsibilities for Medical educators. Simulation-based Medical Education helps fill in these needs.
18: Simulation in Medical education has opened new avenues in teaching:
- Ethical Benefits
- Relevance of Training
- Teach “Error management”
- Teach Safety Culture
- Competency Assessment
- Increased Precision
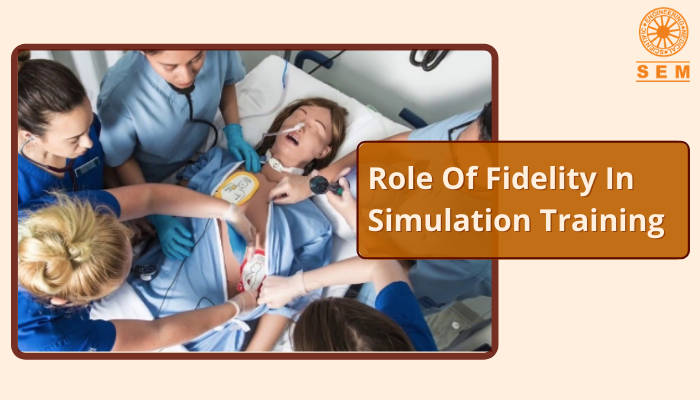
19: Simulation Drills have been used and are widely used in training Emergency Responders and other Care Givers at all levels in Clinical and teamwork skills needed to provide Aid, in Medical Emergencies
20: Simulation allows you to internalize the ramifications of any errors you make and help identify the cognitive processes that led to them.
21: It is well established with overwhelming experimental evidence that one needs repeated and deliberate practice and specific and timely feedback to reach a level of mastery. Simulation helps achieve this much faster and in a more predictable fashion. Residents are able to achieve higher levels of skills earlier in their training.
22: Simulation is very useful and effective in ascertaining competencies. The Core Competencies most conducive to Simulation based training are
23: Simulation is appropriate for Performance Assessment, but there is scarcity of Evidence, that supports the validity of Simulation in the use for Performance Certification.
24: There is current need for standardization and definition in using Simulators for Performance Evaluation
25: Scenarios and tools should be formatted and standardized to enable Reproducibility, Reliability and Validity of data
26: The Institute of Medicine USA estimates that annually
- 44000 to 98000 deaths occur primarily due to “Medical Mistakes” during treatment
- 225000 deaths from Medical errors including 106000 deaths due to non error adverse events of Medical procedures
- 7391 deaths resulted from Medication errors
27: Simulation offers distinct advantages not specifically related to only training
- Less Costly
- Time Efficient
- Less personnel required
- Many automated processes
- Ability to store Performance histories
- Track Global statistics for linked Medical Simulation
- Less medical related accidents
28: Simulation based Training provides a very reliable tool for particularly evaluating Surgical Proficiency. Current Simulation Technologies can reliably measure and demonstrate Resident Competencies in Emergency and Acute Care Management
29: Allows both novices and experienced physicians to practice challenging procedures and learn from their mistakes.
30: Simulation based Medical Training is very particularly valuable in training for scenarios which are rare but high risks events since Caregivers can be confronted with them on training on demand without risk to patient, training for hypothetical high risks situations before they can become a reality
31: Simulation based Training improves Team Performance in Crisis situations wherein Team drills are a natural and effective compliment. Simulation promotes team based Inter-Professional approaches to Learning and to promote Health Care
32: Simulation opens up new vistas for comprehensive planning of skills and educational needs in the Technical and Organizational support structures:
- Helps identify the specific Educational and Training needsLets the needs guide the choice of Facilities and Equipments needed including Simulators
- A Unified Approach provides a tool for comprehensively improving and assessing skill levels of Physicians and other care Givers across the Institution
33: Simulation enables the entire Hospital to engage in exercises that improve:
- Communications
- Provide effective team work even in Crisis situations
- Enhance camaraderie amongst staff
In today’s complex fast paced and stressful Hospital Environments, these benefits of Simulation Training carry a value that’s real and tangible
34: By involving Educators in the fields of Medicine, Nursing, Disaster Management, Emergency Response and the Military, The Medical Profession has succeeded in making a new generation of Medical Simulation Tools that allow for higher levels of preparedness and safety. Medical Simulation has opened up an enormous number of possibilities in the ways to teach.
35: Simulation provides “Elements of Training” without the necessity for a clinical challenge to arrive via the Emergency Room, or for a Simulation to develop in the Hospital and can be done multiple number of times till the Trainee is comfortable and proficiency is reached.
36: Simulation can contain Curriculum and can measure Performance against Established methods.
37: Simulation helps assess individual preparedness to manage an extremely low frequency life threatening event encountered in practice, example, “Recognition and Management of Severe Reactions to Iodinated Contrast Materials in Children of differing ages and sizes in Radiological Examinations”, e.g., “Recognition and Management of Malignant Hyperthermia.”
38: Rarity of an Emergency guarantees an uneven training experience across a large number of residents . To render training more homogenous it is necessary to standardize the Training and incorporate it and adopt specific simulated clinical scenarios into the Training curriculum. This means that not only assessing trainees, but also training them with it to guarantee that each Resident reaches specific milestones.
39: Simulation helps in acquiring skills far away from the patient as possible (it is about respect). Learning Clinical Skills in a “Low Stakes Environment” satisfies one of the three fundamental principles (Primacy of Patient welfare) and one of the Ten professional responsibilities (Commitment to Professional Competence) of the “Physician Charter on Medical Professionalism in the New Millennium” drafted by the “American Board of Internal Medicine Foundation, The American College of Physicians, American Society of Internal Medicine Foundation, and the European Federation of Internal Medicine, endorsed by the American Board of Radiology and the Radiological Society of North America.
40: Simulation Labs can foster:
- Critical Thinking
- Communication Skills
- Teamwork necessary to function successfully in that environment.
Students develop higher order Cognitive Skills and gain opportunity to acquire and refine Cognitive, Technical and behavioral skills by solving complex Multidimensional problems in an environment without the risk to patients.
41: Students needing remediation in Clinical Skills can greatly benefit from Simulation Scenarios.
42: Realistic Educational experiences that give students the chance to hone skills before working on real patients is more important than ever
43: In the USA and now also in India, it is increasingly difficult to place students in certain types of Clinical settings such as Pediatric and Maternal and Obstetrical Units because of Liability concerns. Simulation Training can go a long way in compensating for this limitation.
44: Simulation has effected a decisive shift of focus from knowledge acquisition to the acquisition of defined levels of acceptable clinical performance.
45: Simulation has brought within their field of training those healthcare procedures that are potentially dangerous and which are very difficult to teach and learn.
46: Simulators have decisively done away with the current paradox in the Healthcare System, i.e. “Today’s patients can be harmed in the training of tomorrow’s practitioners”
47: Simulators benefit not only inexperienced and vulnerable Healthcare workers in the start of their careers, but also experienced practitioners learning new procedures.
48: Simulators are valued for their ability to create conditions that optimize learning.
49: Intricate elements of a difficult procedure can be selectively rehearsed again and again.
50: Simulators can be programmed to provide training on patient complications and equipment malfunctions which require decisive action and skilled performance when they occur
51: Simulators enable a complex mosaic of multiple skills- Cognitive, Perceptual, Motor and Affective Skills to be simultaneously exercised.
52: Simulators serve as “Evaluation and Usability” test beds to work out unanticipated wrinkles of new emerging technologies for example :
- Reduced time for training.
- Pressure to reduce costs in the OR.
- New developments and more complex procedures.
- Patient safety.
- Resistance to use Animals and Cadavers-Legal, Ethical and Financial issues- Animals and cadavers have no feedback or assessment and cannot incorporate scenarios of various pathologies.
- Simulators offer targeted, self directed, autonomous, individually focused training.
- Simulation technologies have inherent Structural Replicable Learning Experiences, that can build on prior experiences, resources and mental models.
Within this structure, Users can adopt the content and complexity of their experience to meet their defined needs.
53: Structured tasks meet an important requirement for effective adult learning. Adults when learning need to know:
- Why they are learning something
- What they are about to learn
- How they are going to learn it.
Simulators effectively meet adult learning needs.
54: Simulators are essentially an Action Learning Experience, but with Multi Media capabilities, they offer a complete set of Conceptual Knowledge, Sensory Knowledge and Error Avoidance Comprehensive Feedback.
55: Simulators deliver Objective Assessment of Learning Needs, thereby intrinsically motivating the learner to readily accept gaps in his/her Knowledge and Skills
56: Simulation Centers offer what a single mannequin cannot, i.e. “A realistic and versatile setting to train in an environment in which Physicians, Nurses and staff can fine tune the Cooperation and Team Work and speed needed to respond effectively to the reactions of the patients, that mannequins replace.
57: Simulators do not become tired or embarrassed or behave unpredictably (as real or ill patients may) and therefore they provide a standardized experience for all trainees.
58: Mastery of Clinical Tasks involving innovative Diagnostic and Therapeutic technologies for example deployment of medical devices via Minimally invasive or endovascular techniques, often follow a steep learning curve with
As technologies improve and newer ones are adopted, newer learning techniques and methodologies will evolve simulators with greater anthropomorphic characteristics and realistic human responses to a variety of clinical presentations.