Trauma Manikins – Surgical Procedures Involved & Application
Traumatic injuries have a great chance of becoming the third-largest cause of death around the world. Trauma is no different than any other illnesses and injuries that arise anywhere near the top ten list. The people working in emergency care make constant efforts to improve the care provided to traumatic patients. For that many other metrics have also been added for them as an evolution of care.
In a dynamic condition, patients can be treated with the help of healthcare simulation. Also, medical simulation is used to deliver, record and assess the applications of life-saving interventions and treatments in a high frequency and low consequence environment. This has resulted in the development of a class of manikins that are called ‘Trauma Manikins’.
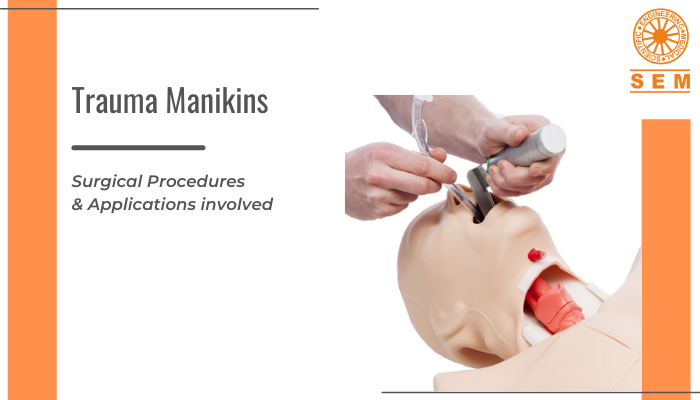
Introduction To Trauma Manikins
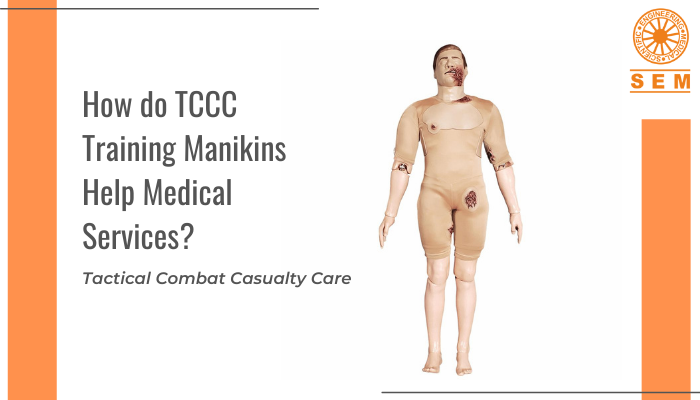
Trauma Manikin is a surgical simulation manikin used for medical professionals, to teach them surgical skills, including the American College of Surgeons’ Advanced Trauma Of Life Support (ATLS) program. At the time of combat situations, advanced surgical skills training is provided through Trauma Manikins. These surgical trainers are preferably used at the place of a simulation trainer by both instructor and medical students for teaching emergency trauma surgical skills.
As for any manikin-based clinical simulation, there are many manufacturers that design ‘Trauma Manikins’ based on the traumatic situation they are going to be used for the demonstration. The educators and administrators have a tendency to pick a manikin that has the label ‘Trauma Care’ as according to them, that particular kind must be the best to meet their individual needs. Not only this, but there are some manikins which are specially endorsed by different organisations to be the only manikin that is suitable comprehensively for a specific course. As it becomes important for the instructors to have the specific manikins for the specific courses and not the ones that do not meet their needs.
Surgical Procedures
Basically, a ‘Trauma Manikin’ can be used to simulate the needed experience or skill set of a particular profession which is related to the care that a medical professional is considered to deliver in a scenario that involves traumatic injury. These manikins may include any or all of the following simulation healthcare capabilities and are used to train on the following surgical procedures:
- Cricothyrotomy
- Percutaneous tracheostomy
- Needle decompression
- Chest tube insertion
- Pericardiocentesis
- Diagnostic peritoneal lavage
- Intravenous cutdown
- Humans like weight and issues related to musculoskeletal stabilization and transfer
- Articulable head and neck to allow for cervical spine manipulation and immobilization
- Haemorrhage control including exhibiting haemorrhage, ability to cease blood flow with well-aimed direct pressure, tourniquet, or surgical intervention
- Airway intervention including intubation or other advanced airway devices, needle and/or surgical cricothyrotomy, tracheostomy, insertion of NPA and OPA, and other less common airway interventions
- Needle decompression of the chest
- Chest tube maintenance, and monitoring
- Surgical interventions for traumatic injuries
- Various ultrasound examinations
- Simulated open and closed musculoskeletal injuries
- Amputations and various levels of simulated bleeding
- Additional simulation of associated signs and symptoms related to patient presentation after a traumatic injury
- Often these manikins are also “designed or improved to be hard-wearing or shock-resistant” in order to be used in environments that mirror more common points of injury sites.
There are various kinds of manufacturers who have their own way of providing varying degrees of simulated skills through trauma manikins and combinations of the above and other different capabilities to satisfy the demands at different levels of providers.
Some specific examples that do not include trainers but only consist of manikins that are specifically built for traumatic situations, being different from other manikins that are able to simulate some trauma skills in addition to their normal capabilities:
Nasco Healthcare
- Pericardiocentesis simulator
- Chest drain simulator
- Tension pneumothorax simulator
- Central venous catheterisation simulator
Trucorp company
3B Scientific
OEI tactical casualty simulators
Simulaids
Application in Trauma Simulation
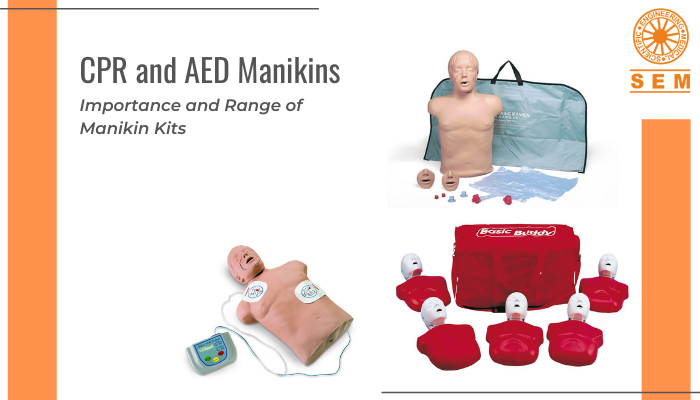
There is a trend both in peer-reviewed literature and in the industry investment in trauma simulation – The capability to simulate the trauma scenarios that are more and more complex and realistic with the use of high fidelity, high technology, manikin based simulation.
This has given rise to the increased usage and coordination of technical and non-technical skills in the delivery of simulated patient care. The function and coordination of this care eventually lead to more research being done on how to accomplish the topmost level of quality and efficiency in the delivery of trauma care.