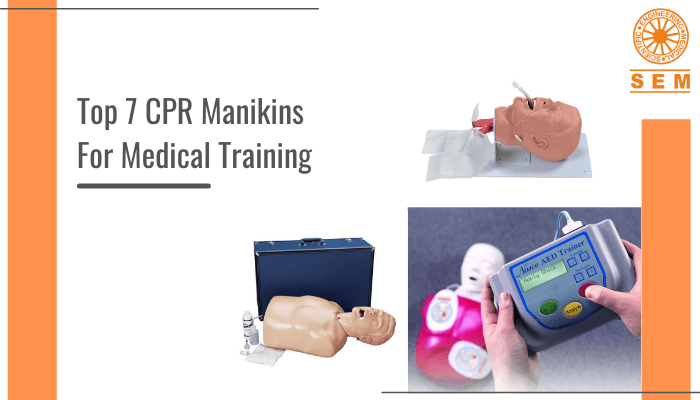
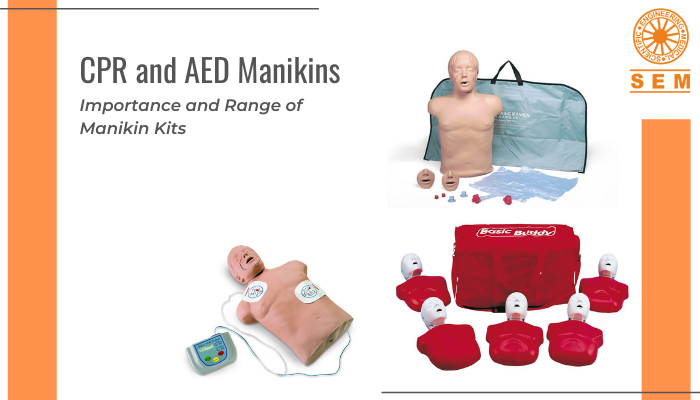
CPR Essentials: You can’t Talk Medical Training Without These 7 CPR Manikins!
Simulation training has changed the way we approach medical training. It has made great strides in training students on Cardiopulmonary Resuscitation (CPR) skills as well. (A rather convenient option to employing the techniques on real actors.) And with something as urgent as CPR, using realistic manikins can mimic performing CPR on a real person. And students learn better when they can believe the scenario and accept it to be happening.
When we use realistic manikins for CPR training, they help students gain vital skills. These manikins often react realistically to certain stimuli. For instance, just by tilting the head or the chin, we can manipulate the airway and simulate choking or obstruction.
As a First-Aid and CPR instructor, CPR manikins will be your biggest investment in medical training. And for the training to be effective, it is important to use high-quality manikins that employ the best trade-off between fidelity and cost. Essentially, these are medical training equipment used to teach advanced medical procedures and CPR. Finding the right manikins for your training program is important and can depend on your needs. But no matter what you are going for, the following 7 manikins are the must-have of any CPR training program, as they are extremely realistic, responsive high-quality manikins that increase efficiency and encourage learning.
BASICBilly+ incl. Upgrade KIT (Adult CPR Torso With Feedback APP)
The BASIC Billy+ BLS and CPR is a pocket-friendly AHA-compliant BLS manikin that works on Bluetooth to let you train, monitor, analyze, and debrief CPR performances while students can learn the correct hand positions for chest compression, pratice resuscitation, and see their own performance in real-time. Through correct cardiac massage and ventilation technique with direct feedback, this manikin is the perfect example of how you can save lives through CPR if done correctly. This one has realistic anatomical landmarks and head-tilt functionality.
CPR Lilly Pro
This one lets you monitor up to 10 trainees at a time and give real-time objective feedback through the CPRLilly app, increasing effectiveness and efficiency of your course. Trainees can also see their performance in real-time. And the LED lights under the neck give direct feedback and indicate the correct compression parameters of depth, release, and rate. This manikin is extremely durable and easy to clean.
Life/form Basic Buddy Plus Convenience Pack powered by Heartisense
Anatomically realistic AHA-compliant CPR manikin with real-time feedback and easy head-tilt/chin-lift for airway. This manikin is simple to assemble and maintain, and enables effective training with apps and sensor kit. With head-/chin-tilt, you have an open airway, and it’s also easy to simulate an obstructed airway. The Xiphoid process also provides anatomical reference points for hand placement and compressions.
Airway Larry with Heartisense
This CPR manikin provides real-time feedback for compressions and ventilations for up to 6 manikins at a time, and comes with apps and a sensor kit that can be attached to a CPR -feedback-lacking manikin.
Life/form AED Trainer with Basic Buddy CPR Manikin
This universal AED trainer can help prepare students for what to do during emergency “shock” and “no shock” situations at the push of a button. There are four training scenarios for manual and hands-free training. This manikin is inexpensive, and the lung/mouth protection systems are disposable, so no risk of cross-contamination!
Life/form NG Tube & Trach Skills Simulator
This realistic simulator helps practice vital tracheostomy skills, gastrointestinal skills through nasal and oral access, and care for patients with respiratory conditions. It perfectly simulates the trachea, esophagus, lungs, stomach, and other landmarks. And if you add methyl cellulose to water, you can simulate mucous-like fluids of a real patient to add to the lungs and stomach.
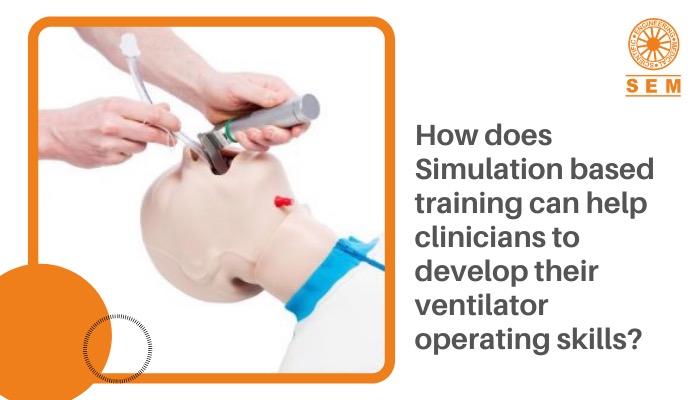
Economy Adult Airway Management Trainer
A detailed adult intubation head so trainees can practice advanced airway management and intubation skills such as endotracheal intubation and nasotracheal intubation, gain anatomy knowledge and recognition, learn to use field emergency airway adjunct tubes like LMAs and Combitube, and learn to secure, suction, and maintain the installation.
These soft, flexible lifesize manikins are an essential in CPR training. The trainee can compress its chest and breathe air into the manikin, learning vital skills along the way, depending on the manikin he is working on. If you are confused about which manikins to get for your CPR training, look no further, because these are the staples of the CPR manikin world.